Hip disease or degenerative disease of the hip joint is one of the most serious diseases of the musculoskeletal system. Because of the larger joint structure, the pain and discomfort are much more severe than when other joints are affected. The pathological consequences are also severe - if the destruction of the small bone joints causes a lot of discomfort, untreated hip arthropathy is a direct route to disability. Only the right treatment, sometimes surgery, can help a person not lose the ability to walk.
What is hip osteoarthritis?
Hip disease, osteoarthritis, hip arthropathy are synonyms for the same pathological process that occurs in one or both thigh areas. In modern medicine, the pathology is also referred to as osteoarthritis: it was previously thought that inflammation is not characteristic of the degenerative process, but more accurate research shows the opposite. Affected articular cartilage tissue releases inflammatory components (interleukins), so osteoarthritis is another correct term.
The disease is characterized by such signs:
- Progress steadily, transitioning from one stage to another,
- causing persistent pain, limited joint mobility,
- Deformation of the bone surface, partial or complete destruction of the hyaline cartilage,
- The late stage is mostly characteristic of the elderly, but it often starts after the age of 40.
- 70% of people over the age of 75 have pathological symptoms,
- Women are more prone to the disease.

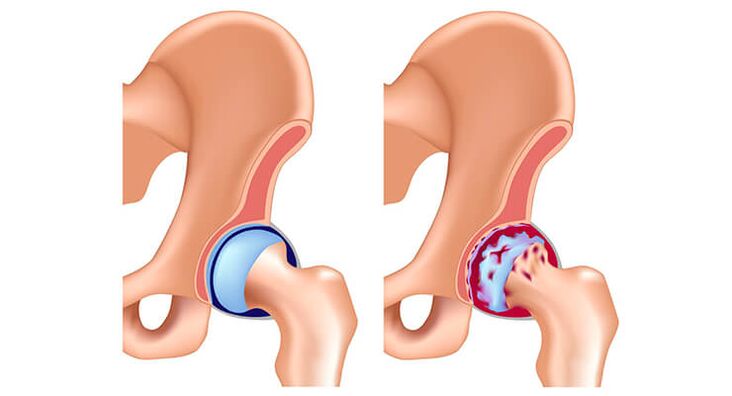
A joint is a mechanism that has friction parts in it. Contact surfaces wear due to a decrease in the quality or quantity of lubrication (inter-articular fluid). Small cracks appear in the cartilage and later they are destroyed, instead of healthy tissue, callus appears. This growth does not allow the leg to move normally and its function is lost.
Cause of disease development
Arthropathy in the right thigh or left thigh area can be primary or secondary, with the first option being typical of older adults. The primary form of the disease develops over decades and is associated with age-related wear and tear and cartilage destruction.
There are other causes of secondary hip disease and can even start in young adults. It is associated with the resulting inflammation (infectious, autoimmune), which promotes pathology. Also, the cause may be trauma to the hip (bruises, dislocations, fractures). Other possible causes of minor forms:
- operations on this anatomical region,
- diabetes and other serious metabolic diseases,
- hormonal disorders,
- Congenital, acquired forms of skeletal curvature and displacement,
- hip dysplasia in children
- Acetabular herniation, femoral head necrosis,
- Systemic vascular disease, leading to deterioration of cartilage nutrition,
- Bone tuberculosis, rheumatoid osteoarthritis,
- gout, Purcell disease,
- Tumors are divided into benign and malignant.

Symptoms of any form of hip arthropathy appear more quickly if risk factors are acting on the body:
- constant stress, neurological shocks, depression and worry,
- obese, or even moderately overweight,
- unfavorable genetics,
- Lack of exercise, sedentary work or certain occupations that place a high load on the joints,
- Excessive physical (strength) load, professional sports.
symptoms of disease
The developing hip arthropathy and its symptoms cannot be ignored. Even in its early stages, the disease can make itself feel, especially pain. As the disease progresses from one stage to another, the pain of hip appearance and progressive arthropathy increases. They appear in the thigh area, knees, groin, and even the lower abdomen. Usually after sleep, the pain subsides, but in advanced stages, it may persist. Pain is not always felt on palpation, as joint damage may begin at a deeper location.
Other possible signs of illness:
- A creaking noise when moving, sometimes even slightly,
- limping, changing gait,
- shortening of the leg on the side of the hip joint,
- Stiff movement, limited rotation, leg movement.
As development progresses, other signs of pathology appear. Therefore, palpation gives a feeling of bone deformation, with a feeling of growth. During the examination, doctors noticed muscle atrophy and the patient, even in daily life, was forced to move on crutches, crutches due to pain and weakness in the limbs.

In general, pain and other clinical manifestations are highly dependent on stage. Hip disease has the following stages:
- first.Symptoms are mild, but initial changes are already evident during diagnosis. The synovial fluid thickens and decreases in volume, and the cartilage structure changes at the end of the stage. Small cracks appear and the body tries to heal these cracks by forming small "corns".
- second.The pain is quite obvious at this stage, crunching, and the motor function is obviously limited. Pain syndrome can radiate to other parts of the body and spread throughout the leg. The picture shows: thinning of the cartilage, narrowing of the distance between the bones, destruction of the structures of the articular surfaces, and sometimes - displacement of the bones from the cavity. Increased number of bone growths (osteophytes).
- third.The pain becomes unbearable, a person's movement is severely restricted, and many stop moving altogether. The cartilage is almost completely destroyed, the muscles atrophy, and the joints are severely deformed. Osteophytes look like spikes and can irritate nerve endings.
What are the risks and complications?
It is easy to understand that for a condition such as hip arthropathy, if the symptoms and treatment are not properly identified and not timely, this will threaten disability. Severe pain syndrome, inability to walk, needing constant care - that's what's waiting for someone who doesn't have treatment for this condition.
Based on the severity of the disease, disability when the thigh bones were damaged, with no job opportunities at all, they gave to the first group. Surgery on such patients - this is the only effective treatment in this condition. But even modern methods of operation can carry a risk of complications:
- contagious infection,
- thrombosis, thromboembolism,
- Massive blood loss.

The overall rate of complications is small - 0. 5-2%, but they do occur. In most cases, the prosthesis becomes infected and must then be replaced with a new one. That's why it's important to give antibiotics after surgery.
Diagnosis of joint disease
It is recommended to seek help from a surgeon, surgeon, orthopaedic surgeon at the first signs of injury in the femoral area. Initially, if a hip joint is suspected, a doctor will perform a physical examination:
- Feel the upper thigh, showing pain points, osteophytes,
- Perform passive leg movements - flexion, extension, abduction and adduction to determine the possible range of motion.
Instrumental diagnosis will help to make more accurate diagnosis and treatment of hip arthropathy. Usually radiography - the cheapest, available research method. X-rays are recommended on modern equipment, or replaced with CT scans, which have much higher image quality. CT provides comprehensive information on bone, cartilage, and joint surface conditions. If a detailed study of a soft tissue condition is required (for example, when a nerve root is pinched), a specialist will prescribe an MRI.

Other possible diagnostic measures:
- joint ultrasound,
- arthroscopy,
- blood test for rheumatoid factor,
- tuberculin test,
- Biochemical analysis of suspected diabetes and gout.
Finding the cause of secondary hip disease is very important because it is impossible to stop the progression of the disease without affecting it.
Treatment of Hip Arthropathy - Medications and Physiotherapy
If the signs of the disease are insidious and the stage of irreversible change has not been reached, conservative treatment will help the patient. When hip arthropathy becomes severe, medication is also required—as part of the treatment process.
How to treat hip joint disease? There is a plan for medication to correct the disease:
- Non-steroidal anti-inflammatory drugs. Pills or injections will help eliminate pain and inflammation. They cannot be used uncontrollably - the cartilage's own ability to regenerate is reduced, and the stomach and intestines can be severely affected by NSAIDs.
- Vascular drugs. Treating with this method helps to strengthen the cartilage's nutrition and aid in its recovery.
- Muscle relaxant. For muscle spasm pain caused by damage to the thigh area.
- chondroprotective agent. Osteoarthritis of the hip requires mandatory use of these drugs for several months. Injectable forms are also required to be applied in the course, including injection into the joint cavity. A more effective technique is to introduce hyaluronic acid preparations into the joints.
- corticosteroids. In extreme cases it is used as an intra-articular injection. This treatment is necessary if symptoms become unbearable.

Topical medications (ointments, gels) used to treat hip arthropathy are often ineffective due to the deep joint location. But physical therapy techniques are often used and can provide serious pain relief. UHF, laser therapy, magnetic therapy is performed on the thigh area, UHF, massage is performed. Also, with osteoarthritis, manual treatment is required, and in some cases - joint distraction.
Folk remedies for arthritis
Although hip arthropathy does not respond well to various external methods, many people use alternative therapies to treat the disease. Insulating compression should only be used on the painful area if there is an intense pain syndrome, although it will be more distracting. Oral medications are best used to treat complex and advanced hip arthropathy:
- Pour 100 grams of dried clover with 500 ml of vodka, in the dark for 10 days, take 30 drops 3 times a day to reduce inflammation,
- Make jelly every day, and in the absence of contraindications, prepare jelly regularly - dishes will not be worse than chondroprotectants.
You can reduce pain with the help of this compression. It is necessary to mix equal amounts of honey, medicinal bile, ammonia water, and glycerin, apply it to the joints, and tie it with a hot cloth. Leave the compress on for 3 hours, then rinse off.

Other methods and actions
For comprehensive osteoarthritis treatment, following the right diet is very important, and you will have to give up foods that disrupt your blood supply and damage cartilage nutrients. These are bacon, vinegar, salty foods, fried foods, and foods that contain preservatives, trans fats. But the diet should eat more dishes containing magnesium, potassium, iodine and calcium.
Essential to the treatment of hip arthropathy is therapeutic exercise. All patients should perform daily warm-up, specific exercises in the supine position. For example, you need to slowly lift your leg and hold it above the floor for a few seconds. It is important to rule out sudden movements and avoid prolonged brisk walking - in the case of hip joint disease, this will only increase the progression of the disease. To unload the joint, you can use a cane, crutches, or an orthopaedic surgeon can recommend special orthoses to lighten the load.
Third, the treatment of end-stage hip joint disease can only be carried out by means of surgery, and other methods are ineffective. In 95% of cases, the surgery is successful and leg movement is fully restored. But prosthetics are not permanent, with a lifespan of up to 20 years, so surgery is a last resort. In an arthroplasty, your own joint is replaced by an artificial one, and the arthropathy of the hip no longer threatens him.

Prevent hip disease
In order not to undergo complex pathological treatment and not to suffer from pain syndrome, it is important to start preventive measures from an early age. Prevention of hip disease is especially important for people exposed to risk factors.
In order not to affect the blood supply to the cartilage, you should:
- Include plant-based foods, plenty of lean meats, cottage cheese, jelly, kefir foods,
- Quit smoking, don't drink alcohol,
- sedentary work, regular warm-ups, simple exercise,
- Give up a sedentary lifestyle and switch to low-intensity aerobic activities like skiing, swimming, etc.
In order for a person to not suffer from hip arthropathy, a person should control their weight, prevent obesity, and even gain 5-10 pounds of extra weight - which can seriously increase the load on the femoral area. Hip disease can only be prevented through an integrated approach and a healthy lifestyle!




























