The most common cause of low back pain is spinal disease, mainly degenerative dystrophy (osteochondrosis, spondylotic deformity) and back muscle overwork. In addition, various diseases of the abdominal cavity and small pelvis, including tumors, can cause the same symptoms as intervertebral disc herniation, compressing the root of the spinal cord.
These patients will not only turn to neurologists, but also to gynecologists, orthopedics, and urologists. Of course, the most important thing is to turn to local or family doctors. This is no coincidence.
The etiology and pathogenesis of low back pain
According to modern concepts, the most common causes of low back pain are:
- Pathological changes of the spine, mainly degenerative malnutrition;
- Pathological changes of muscles, the most common is myofascial syndrome;
- Pathological changes of abdominal organs;
- Nervous system disease.
The risk factors for low back pain are:
- Heavy physical activity;
- Uncomfortable working posture;
- Injured;
- Cool down, draft;
- Abuse of alcohol;
- Depression and stress;
- Occupational diseases related to exposure to high temperatures (especially in hot shops), radiant energy, severe temperature fluctuations, and vibration.
The vertebral causes of low back pain include:
- Root ischemia (discogenic radiculopathy syndrome, radiculopathy), caused by a herniated disc compressing the root;
- Reflex muscle syndrome, which may be caused by degenerative dystrophic changes in the spine.
Various dysfunctions of the lumbar spine, when the intervertebral joint block appears due to incorrect posture, and its mobility is impaired, it has a certain effect on the occurrence of low back pain. In the joints above and below the block, compensatory hyperactivity occurs, causing muscle spasms.
Signs of acute compression of the spinal canal
- Perineal numbness, weakness and numbness in the legs;
- Delayed urination and bowel movements;
- As the spinal cord was compressed, pain relief was observed, and numbness of the pelvic girdle and limbs alternated.
Low back pain in children and adolescence is most often caused by abnormal spinal development. 20% of adults will have non-overgrowth of the vertebral arch (spina bifida). Examination revealed hyperpigmentation, birthmarks, multiple scars and hyperkeratosis of the waist skin. Sometimes there will be urinary incontinence, nutritional disorders, and leg weakness.
Low back pain can be caused by lumbar vertebralization (the transition of the S1 vertebra relative to the lumbar spine) and sacralization (the connection between the L5 vertebra and the sacrum). These abnormalities are due to the individual characteristics of the development of the transverse process of the vertebrae.
Classification form
Almost all patients complain of back pain. The disease is mainly manifested by inflammation of sedentary joints (intervertebral joints, costal joints, lumbosacral joints) and spinal ligaments. Gradually, their ossification develops, the spine loses elasticity and functional mobility, and becomes like a bamboo pole, fragile and easily injured. At the stage of obvious clinical manifestations of the disease, the mobility of the chest and the lung capacity of the lungs significantly decrease during breathing, which will lead to the development of many lung diseases.
Spinal tumors
Distinguish between benign and malignant tumors, mainly originating from spinal and metastatic benign spinal tumors (osteochondroma, chondroma, hemangioma) and sometimes clinically asymptomatic. For hemangioma, spinal fractures may occur even with minor external influences (pathological fractures).
Malignant tumors, mainly metastatic, originate in the prostate, uterus, breast, lung, adrenal glands and other organs. Pain in this situation is more frequent than benign tumors-usually continuous, painful, and can be exacerbated by slight movements, depriving the patient of rest and sleep. It is characterized by a gradual deterioration of the disease, increased overall fatigue, and obvious changes in blood. Very important for diagnosis is radiography, computed tomography, and magnetic resonance imaging.
Osteoporosis
The main cause of the disease is due to an independent disease or the decline in the function of the endocrine glands under the background of general body aging. Osteoporosis can occur in patients who take hormones, chlorpromazine, anti-tuberculosis drugs, and tetracycline for a long time. Nerve root disease that accompanies back pain is caused by deformed intervertebral foramina and spine (myelopathy)-due to compression of the nerve root medullary artery or vertebral fracture, even after minor injuries.
Myofascial syndrome
Myofascial syndrome is the main cause of back pain. It can occur due to overwork (during heavy physical exertion), hyperextension and muscle bruising, non-physiological posture during work, response to emotional stress, shortening of a leg, or even flat feet.
Myofascial syndrome is characterized by the presence of so-called "trigger" areas (trigger points). Pressure causes pain and usually radiates to adjacent areas. In addition to myofascial pain syndrome, inflammatory muscle disease-myositis can also cause pain.
Low back pain is often accompanied by visceral diseases: gastric ulcer and duodenal ulcer, pancreatitis, cholecystitis, urolithiasis, etc. They can be obvious and mimic the symptoms of low back pain or discogenic lumbosacral radiculitis. However, there are also significant differences, so reflex pain can be distinguished from pain caused by peripheral nervous system diseases caused by underlying disease symptoms.
Clinical symptoms of low back pain
In most cases, low back pain occurs between 25-44 years of age. Distinguish acute pain, which usually lasts 2-3 weeks, sometimes as long as 2 months. And chronic-more than 2 months.
Compressive radiculopathy (discogenic radiculopathy) is characterized by a sudden onset, usually after heavy lifting, sudden exercise, and hypothermia. The symptoms depend on the location of the lesion. The core of the syndrome is the compression of the intervertebral disc on the tooth root, which is caused by the malnutrition process. Static and dynamic load, hormonal imbalance, trauma (including microtrauma of the spine) promote the malnutrition process. In most cases, the pathological process involves the area of the spinal cord from the dura mater to the intervertebral foramen. In addition to herniated intervertebral disc, bone growth, cicatricial changes in the epidural tissue, and hypertrophic ligamentum flavum may also be related to root trauma.
The upper lumbar roots (L1, L2, L3) are rarely affected: they do not exceed 3% of all lumbar nerve root syndromes. The frequency of L4 root involvement increased twice (6%), leading to characteristic clinical manifestations: slight pain along the inner and anterior surface of the thigh, and the inner surface of the lower leg, and paresthesias (numbness, burning sensation, reptiles) in thisArea; slight weakness of quadriceps. The knee reflex persists and sometimes even increases. L5 roots are most commonly affected (46%). The pain is located in the waist and buttocks area, along the outer surface of the thigh, the front outer surface of the calf, to the feet and III-V fingers. It is usually accompanied by skin sensitivity on the front and outer surfaces of the legs and a decrease in the strength of the III-V finger extensors. The patient has difficulty standing on the heel. With long-term radiculopathy and tibial anterior muscle atrophy, the S1 root is often affected (45%). In this case, the pain in the lower back radiates along the outer back surface of the thigh, the outer surface of the calf, and the foot. Examination usually reveals a decrease in pain on the posterior outer surface of the leg, and a decrease in the strength of the triceps and toe flexors. It is difficult for such patients to stand on their toes. The Achilles tendon reflex is weakened or disappeared.
Lumbar reflex syndrome
It can be acute and chronic. Acute low back pain (LBP) (low back pain, "back pain") occurs within minutes or hours, usually due to clumsiness and sudden onset. Tingling, shooting (such as electric shock) throughout the lower back, sometimes radiating to the iliac area and buttocks, increases sharply with coughing and sneezing, and decreases in the supine position, especially if the patient finds a comfortable posture. Restriction of lumbar spine movement and tight psoas muscles cause Lasseger symptoms, often bilateral. Therefore, the patient lies on his back with his legs extended. The doctor bends the affected leg at the knee joint and hip joint at the same time. This does not cause pain, because in this position of the leg, the diseased nerve is relaxed. The doctor then bends the leg at the hip-hip joint and begins to straighten it at the knee, which causes tension in the sciatic nerve and produces severe pain. Acute low back pain usually lasts 5-6 days, sometimes shorter. The first attack ends faster than subsequent attacks. Recurrent episodes of low back pain often develop into chronic PB.
Atypical back pain
Many clinical symptoms are atypical symptoms of back pain caused by spinal degenerative dystrophy or myofascial syndrome. These signs include:
- The appearance of pain in childhood and adolescence;
- Injured back shortly before the onset of back pain;
- Back pain with signs of fever or poisoning;
- spine;
- Pain in rectum, vagina, legs, belt;
- The relationship between low back pain and eating, defecation, sexual intercourse, and urination;
- Neuropathology in the context of back pain (amenorrhea, dysmenorrhea, vaginal discharge);
- Increase in lower back pain in the horizontal position and decrease in the vertical position (Razdolski symptom, characteristic of spinal tumor process);
- The pain lasts for one to two weeks;
- The appearance of limbs and pathological reflexes.
investigation method
- External examination and palpation of the waist to detect scoliosis, muscle tension, pain and trigger points;
- Determine the range of motion of the lumbar spine and the area of muscle atrophy;
- Neurological status study; to determine tension symptoms (Lassegh, Wasserman, Neri). [Wasserman symptom study: knee flexion in prone position causes hip pain. Research on Neri's symptoms: A patient with upright legs and supine bends his head sharply toward the chest, causing acute pain in the lower back and sciatic nerve. ];
- Study sensitivity, reflex bulbs, muscle tone, autonomic disorders (swelling of the skin, changes in color, temperature and moisture);
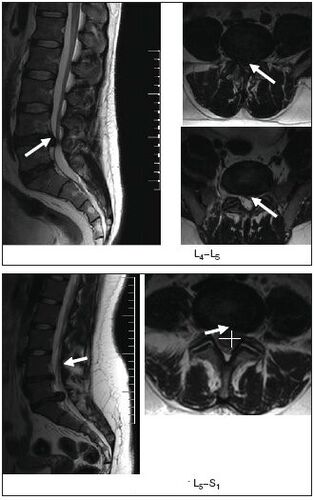
- Radiography, computer or magnetic resonance imaging of the spine.
MRI is particularly informative.
- Ultrasound examination of pelvic organs;
- Gynecological examination;
- If necessary, perform additional studies: cerebrospinal fluid, blood and urine, sigmoidoscopy, colonoscopy, gastroscopy, etc.
treatment
Acute low back pain or worsening of spine or myofascial syndrome
No discrimination. Gentle motor mode. The pain was severe in the first few days, rested in bed, and then walked on crutches to relieve the spine. The bed should be strong and a wooden board should be placed under the mattress. In order to keep warm, it is recommended to use wool shawls, electric heating pads, hot sand bags or salt bags. Ointment has beneficial effects: finalgon, tiger, capsaicin, diclofenac, etc. , as well as mustard plaster and pepper plaster. The recommended dose of erythema is ultraviolet radiation, leeches (taking into account possible contraindications), and the painful area is flushed with ethyl chloride.
The anesthesia effect is provided by electrotherapy: transcutaneous electrical analgesia, sinusoidal modulation current, rheological current, nocaine electrophoresis, etc. Reflex therapy (acupuncture, laser therapy, moxibustion) is effective; nocaine block, trigger point pressure massage.
Medications include analgesics, non-steroidal anti-inflammatory drugs; tranquilizers and/or antidepressants; drugs that reduce muscle tension (muscle relaxants). If arterial hypotension occurs, tizanidine should be used with caution because it has the effect of lowering blood pressure. If swelling at the root of the spinal cord is suspected, a diuretic is prescribed.
The main analgesics are non-steroidal anti-inflammatory drugs, and patients often use them uncontrollably when the pain worsens or recurs. It should be noted that long-term use of non-steroidal anti-inflammatory drugs and analgesics will increase the risk of complications of such treatments. Currently, there are a large number of non-steroidal anti-inflammatory drugs to choose from. For patients with spinal pain, diclofenac 100-150 mg/day is preferable to "non-selective" drugs in terms of availability, efficacy and the possibility of side effects (gastrointestinal bleeding, dyspepsia). Internal, intramuscular, rectal, topical, ibuprofen and ketoprofen 200 mg and topical, from "selective"-meloxicam 7. 5-15 mg/day, nimesulide 200 mg/day.
In the treatment of non-steroidal anti-inflammatory drugs, side effects may occur: nausea, vomiting, loss of appetite, upper abdominal pain. Possible ulcerative effect. In some cases, ulcers and bleeding may occur in the gastrointestinal tract. In addition, headaches, dizziness, drowsiness, allergic reactions (rash, etc. ) were also noted. This product is forbidden to treat gastrointestinal ulcer disease, pregnancy and lactation. In order to prevent and alleviate the symptoms of indigestion, it is recommended to take non-steroidal anti-inflammatory drugs and drink milk during or after meals. In addition, as has been observed in the long-term treatment of many chronic diseases, the combined use of NSAIDs with increased pain and other drugs used by patients to treat concomitant diseases can lead to decreased treatment compliance, and therefore, the treatment effect is insufficient.
Therefore, modern conservative treatment methods include mandatory use of drugs that have cartilage protection, cartilage stimulating effects and have better therapeutic effects than non-steroidal anti-inflammatory drugs. The drug Teraflex-Advance fully meets these requirements and can replace NSAIDs in the treatment of mild to moderate pain syndromes. One capsule of Teraflex-Advance drug contains 250 mg of glucosamine sulfate, 200 mg of chondroitin sulfate and 100 mg of ibuprofen. Chondroitin sulfate and glucosamine are involved in the biosynthesis of connective tissues, helping to prevent cartilage destruction and stimulate tissue regeneration. Ibuprofen has analgesic, anti-inflammatory and antipyretic effects. The mechanism of action is due to the selective blocking of cyclooxygenase (COX type 1 and type 2), the main enzyme in the metabolism of arachidonic acid, resulting in a decrease in prostaglandin synthesis. The presence of non-steroidal anti-inflammatory drugs in the Teraflex-Advance formulation helps to increase the range of motion of the joints and reduce morning stiffness of the joints and spine. It should be pointed out that according to R. J. Tallarida et al. , the presence of glucosamine and ibuprofen in Teraflex-Advance provides a synergistic effect for the analgesic effect of the latter. In addition, the analgesic effect of the glucosamine/ibuprofen combination is 2. 4 times the dose of ibuprofen.
After the pain is relieved, it is reasonable to switch to Teraflex containing the active ingredients chondroitin and glucosamine. Teraflex is taken 1 capsule 3 times a day. In the first three weeks and 1 capsule 2 times/day. In the next three weeks.
In the vast majority of patients, when taking Teraflex, the relief of pain syndrome and the reduction of neurological symptoms are positive. The patient tolerated the drugs well, and no allergies were found. The use of Teraflex in spinal degenerative dystrophy is reasonable, especially in young patients, whether in combination with NSAID or as a monotherapy. When used in combination with non-steroidal anti-inflammatory drugs, the analgesic effect is twice as fast, and the demand for therapeutic doses of non-steroidal anti-inflammatory drugs is gradually reduced.
In clinical practice, for diseases of the peripheral nervous system, including those related to spinal osteochondrosis, B vitamins with neurotrophic effects are widely used. Traditionally, alternate administration of vitamins B1, B6 and B12, 1-2 ml is used. Alternate intramuscular injections every day. The course of treatment is 2-4 weeks. The disadvantages of this method include the use of small doses of drugs that will reduce the therapeutic effect and the need for frequent injections.
For radiculopathy of intervertebral disc, traction therapy is used: traction in the neurology hospital (including underwater), local treatment (nocaine block, ethyl chloride flushing, anesthetic ointment) when myofascial syndrome occurs, the musclesApply hot compresses for several minutes.
Chronic low back pain of vertebral origin or myogenic origin
If the intervertebral disc is herniated, it is recommended:
- Wearing a rigid corset of the "weight lifting belt" type;
- Eliminate sudden movements and tilts and restrict physical activity;
- Physiotherapy exercises to create muscle corsets and restore muscle mobility;
- massage;
- Nocaine blockers;
- Reflexology
- Physical therapy: ultrasound, laser therapy, hyperthermia;
- Intramuscular vitamin therapy (B1, B6, B12), multivitamin and mineral supplements;
- For paroxysmal pain, carbamazepine is prescribed.
Non-drug treatment
Although there are effective conservative treatments and dozens of techniques, some patients still require surgical treatment.
The indications for surgical treatment are divided into relative indications and absolute indications. The absolute indication for surgical treatment is the development of coccygeal syndrome, the presence of isolated disc herniation, and obvious radicular pain syndrome. Despite the treatment, this symptom did not decrease. The development of nerve root spinal cord ischemia also requires emergency surgical intervention. However, after the first 12-24 hours, the surgical indications in this case become relative, firstly, due to irreversible changes in root formation, and secondly, because ofIn most cases, in the course of treatment and rehabilitation measures, the process subsides within about 6 months. The same regression period was observed in the delayed operation.
Relative indications include ineffective conservative treatment and recurrent sciatica. The duration of conservative treatment should not exceed 3 months. And last at least 6 weeks. Assuming that in the case of acute nerve root syndrome and conservative treatment ineffective, the surgical method is reasonable within the first 3 months. Prevent chronic disease root changes after the onset of pain. A relative indication is the extremely obvious pain syndrome, when the pain component changes with the increase of neurological deficits.
From the perspective of physical therapy procedures, electrophoresis of the proteolytic enzyme calipazil is currently widely used.
As we all know, physical therapy and massage are part of the comprehensive treatment of patients with spinal diseases. The goal of therapeutic gymnastics is to comprehensively strengthen the body, improve efficiency, improve coordination of movements, and enhance physical fitness. At the same time, special exercises are designed to restore certain motor functions.




























